Select language
Select language
Welcome to the traditional health worker (THW) resources page for Columbia Pacific CCO providers. A traditional health worker is a person who has similar life experiences with the people they work with. They can assist members in getting services and care that support their health and wellbeing by helping with things like:
There are five types of THWs licensed in Oregon:
THWs can be found in community-based organizations and in primary care and behavioral health clinics. They are a free benefit to members and do not require a referral or prior authorization from Columbia Pacific. However, organizations with THWs may have their own referral requirements to access care. Not all THWs are contracted with Columbia Pacific or provide services to Medicaid Members. To learn more about your THW network and access for Columbia Pacific members you serve, contact your regional THW Liaison listed below.
The OHA Office of Equity and Inclusion has identified Best and Promising Practices & Other Resources for THWs. This information is available on the OHA-OEI THW website:
oregon.gov/oha/OEI/Pages/Information-for-Health-Systems,-Providers,-and-THW%27s.aspx
Please direct questions related to THWs to: colpacthwliaison@careoregon.org
For an outline of the process and covered benefits for doulas interested in serving Columbia Pacific members, view our Columbia Pacific CCO doula coverage FAQ
For the most current guidance in billing, view the 2025 OHA Birth Doula Fee-for-Service (Open Card) Billing Guide
Get the details on becoming eligible to bill for THW services, how to submit claims and more:
Columbia Pacific CCO External peer billing guide
Columbia Pacific CCO CHW Billing Guide
Use these documents to assist with integration of THWs into your network:
Columbia Pacific wants to help you and your patients have the best experience, which is why we help you coordinate live interpreters for patients who speak a language other than English. Click here to learn about our resources.
Non-emergent medical transportation to medical appointments is a benefit to OHP members.
NW Rides Ride scheduling: 503-861-0657, toll-free: 888-793-0439, TTY 711
NW Rides is the non-emergent medical transportation (NEMT) program for Columbia Pacific CCO members. It is a benefit through OHP members’ coverage that helps them get transportation services — based on their needs — to their health care appointments including medical, behavioral health and dental appointments.
Members can contact NW Rides to talk about transportation services. Their phone number is 503-861-0657, toll-free: 888-793-0439.
NW Rides is available only for services covered by the Oregon Health Plan. Some appointments may require members to call or get approval before trips can be scheduled. For trips beyond the Columbia Pacific CCO service area, members may need prior authorization to use NW Rides.
Trip requests can be made as many as 30 days or as few as 48 business hours in advance of the transportation need. Same-day and next-day visits may be approved if they are medically necessary and urgent.
NW Rides offers three services:
Check out our Riders Guide for details about the NW Rides transportation program. Feel free to share it with your patients.
If you want printed copies of the Rider's Guide, please contact Columbia Pacific CCO Customer Service at 855-722-8206 or TTY 711. We will send you the printed Rider's Guide within five business days.
When members have health needs that aren’t covered by a health plan or other services, Columbia Pacific CCO offers funds for health-related services (HRS). HRS must be consistent with a member’s treatment plan, as developed by their primary care team or other treatment providers. The services will be documented in the member’s treatment plan and clinical record. For that reason, members without a current provider relationship need to establish one in order to receive health-related services funds.
Providers who would like to learn more about the basic framework of Health-Related Services flex process, regulatory requirements and how to access this resource, please watch this webinar by clicking here.
These funds cover items or services that aren’t covered under standard health plan services but will improve a person’s health. Health plans cover provider visits, pharmacy benefits and durable medical equipment. Durable medical equipment (DME) is a covered benefit, which means equipment that would be covered as DME is not eligible for HRS funds. (For a list of items covered by DME with no authorization required, click here.)
Health-related services funds cover services like:
This is not an exhaustive list. Any requested items will be evaluated for consistency with a member’s health needs and treatment plan.
Limitations of health-related services: The Oregon Administrative Rules restrict health-related services to items not paid for with grant money, funding separate from CCO contract revenue, or normal clinical service billing. In other words, health-related services may be used only if other funding is not available. Before you make a request, please be sure there is no other funding available.
Making a health-related services request: Any health care provider, primary care team, care coordination staff member working directly with members, or other subcontractors of Columbia Pacific’s network may request the use of HRS for a member. Columbia Pacific encourages our community-based organization (CBO) partners to help our shared members access HRS. CBOs can work with members and their treatment providers to identify the need, and the provider can submit a request.
All HRS requests must include medical documentation (care plan, progress notes, chart notes, etc.) and information about the member’s diagnosis.
There are two ways to submit requests for health-related services:
Columbia Pacific CCO evaluates all completed request forms based on:
We provide members with a written outcome and copy the requesting provider (and member representatives, if applicable). Often, this involves asking for more information about the member, which may include the member's budget information. Requests cannot be fulfilled until all information is received.
Depending on the nature of the request, if more details about the budget is indicated, this form can be used to provide that information.
Questions? Email us at social.determinants@careoregon.org.
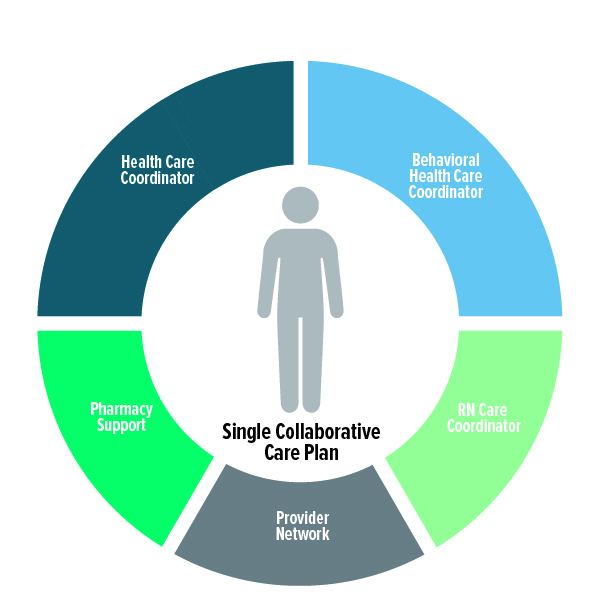
The Columbia Pacific CCO Regional Care Team (RCT) offers providers a community of resources with a single point of contact for you and your patients. The RCT works closely with providers and members – through both telephonic and community-based support – to smooth the way to better care and better outcomes. Click here to view our Regional Care Team overview in PDF format.
With care coordination through the RCT, we will deliver
the right care, at the right time, in the right place, with the right team.
Members will have a consistent care team that will collaborate across disciplines to develop and implement a member-centric care plan through telephonic, electronic or community-based interventions to resolve identified needs and promote healthy outcomes.
The RCT is made up of care coordinators with a variety of backgrounds and experience, including:
Each patient is assigned to a care team that is familiar with the patient’s history, strengths, needs and support system. The team will:
Your dedicated RCT will work closely with your clinic to:
RCTs are assigned based on the county the patient’s PCP clinic is in or the county where the patient lives.
The RCT offers care coordination and support for patients with multiple or complex needs, such as:
Online: Submit a completed Care Coordination Referral form and we’ll route it to your assigned RCT.
Email: Send your completed form to ccreferral@careoregon.org.
Fax: Print and send your completed form to 503-416-3676.
Collective (PreManage): If your clinic uses this online platform, check the RCT tag after searching for your patient.
Call: You can reach your RCT directly at 503-416-3743.
Download a PDF summary of this information here.
This document provides information about dental care benefits for members, including provider options and contact details.
Website feedback
Help us improve our website
Having trouble finding what you’re looking for? Want to tell us about your website experience? Take our feedback survey and let us know!