On this page, you'll find important information about your plan and benefits. Click on a topic below to learn more.
The Columbia Pacific CCO Member Handbook is available in the following languages:
Or read the handbook in large print:
If you would prefer a printed copy of the handbook, call Customer Service at 855-722-8206 (TTY 711). There’s no charge, and you’ll receive a copy within five business days. You may also receive a copy in large print or in languages other than English.
OHP Bridge is a new Oregon Health Plan (OHP) benefit package that covers adults with higher incomes. People who can get OHP Bridge must:
- Be 19 to 65 years old;
- Have an income between 139 percent and 200 percent of the federal poverty level (FPL);
- Have an eligible citizenship or immigration status to qualify; and,
- Not have access to other affordable health insurance.
OHP Bridge is almost the same as OHP Plus.
The two benefit packages are almost the same. There are a few things that OHP Bridge does not cover. To learn more about what OHP Bridge does not cover, please see the table below.
| OHP Bridge covers | OHP Bridge does not cover |
|---|---|
|
|
OHP Bridge is free to members. Just like OHP Plus, OHP Bridge is free to members. That means no premiums, no co-payments, no coinsurance, and no deductibles.
OHP members with income changes may be moved to OHP Bridge automatically. If you have OHP now, you don’t have to do anything to get OHP Bridge. If you report a higher income when you renew your OHP, you may be moved to OHP Bridge.
People who do not have OHP right now can apply for OHP Bridge.
Go to Benefits.Oregon.gov to apply. You can also use that link to find information about how to apply in person, get application help, or to get a paper application. To apply over the phone, call the ONE Customer Service Center at 1-800-699-9075 (toll-free, all relay calls are accepted).
Below is a list of some of the most frequently used forms. Click on a link to open the form in PDF format.
- Direct Member Reimbursement form (prescription drugs)
- Member COVID-19 At Home Test Reimbursement form
- Authorization to Release Personal Health Information (PHI) form
- Member Request to Review Claims Records form
- Appointment of Representative form: English | Spanish
- Complaint and feedback form: English | Spanish
When you become a Columbia Pacific member, we'll mail you a Member ID card within 30 days. Your Member ID card lists your primary care provider (PCP). It also lists important contact information. The card looks like this:
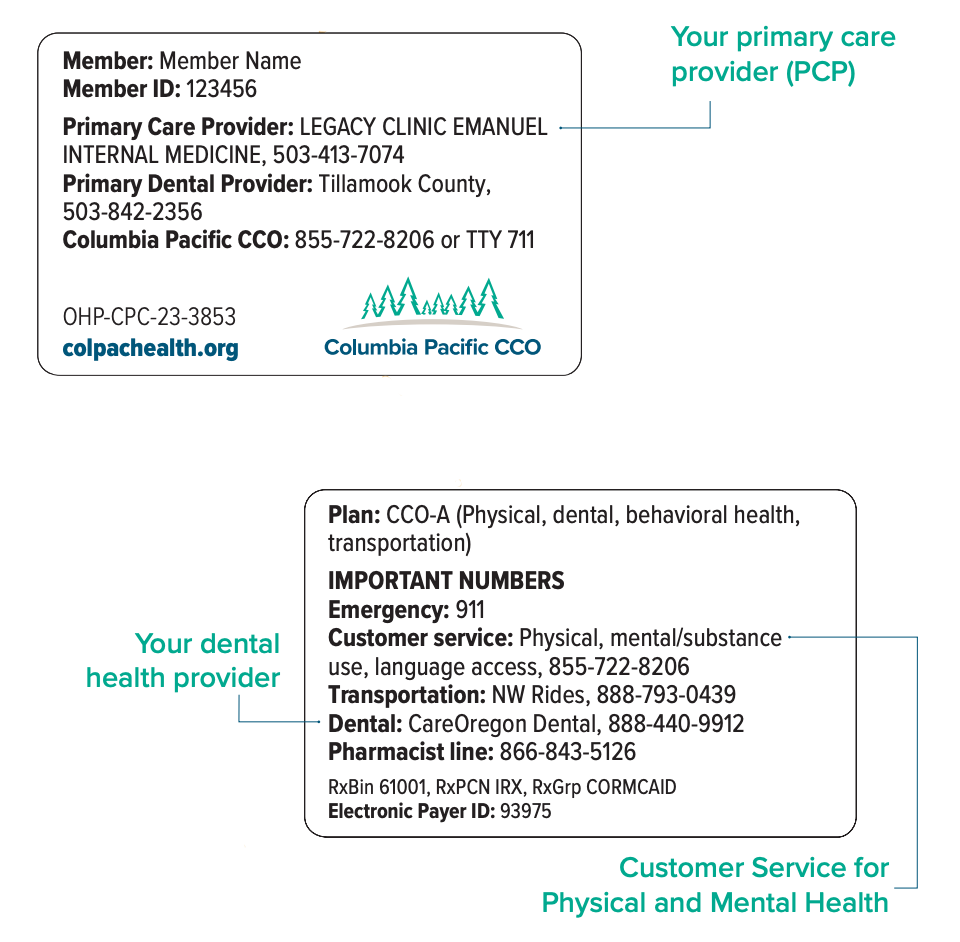
Take your Member ID card and your Oregon Health ID card to all health care and dental appointments and to the pharmacy when you fill a prescription.
Reasons to take your card with you:
- It's easier to check in for appointments.
- It's easier to get medicine at a pharmacy.
- Your provider will know who to bill.
- Providers use information on Member ID cards to make sure you have benefits with us.
If you need an interpreter for visits or phone calls to your (or your child's) provider's office, you are legally entitled to this service free of charge. When you join Columbia Pacific, you may receive a Preferred Language card. This card helps you tell your provider's office about your spoken language. The card shows the preferred language you chose on your insurance application. Show this to your provider to receive interpretation.
For phone interpretation, call our Customer Service when you're at the doctor, dentist or pharmacist or making an appointment.
Call Customer Service if you ask for an interpreter but don't get one. It's important for us to know so we can follow up and improve the process.
As an OHP member, you will be:
- Treated with dignity, respect and privacy.
- Free to choose your primary care provider (PCP).
- Urged to tell your PCP about all your health concerns.
- Able to have a friend or helper come to your appointments. You can also have an interpreter if you want one.
- Told about all your OHP-covered and non-covered treatment options.
- Allowed to help make decisions about your health care, without being kept away from other people or forced to do something you don’t want to do. This includes refusing treatment.
- Given a referral or second opinion, if you need it.
- Given care when you need it, 24 hours a day and seven days a week.
- Free to get mental health and family planning services without a referral.
- Free to get help with addiction to tobacco products, alcohol and drugs without a referral.
- Given handbooks and letters that you can understand.
- Able to see and get a copy of your health records.
- Able to limit who can see your health records.
- Sent a Notice of Action letter if you are denied a service or there is a change in service level.
- Given information and help to appeal denials and ask for a hearing.
- Free from any form of restraint or seclusion (isolation) that is not medically necessary or is used by staff to bully or punish you. Staff may not restrain or isolate you for their convenience or retaliation against you. You have the right to report violations to Columbia Pacific CCO and/or the Oregon Health Plan.
- Allowed to make complaints and get a response without a bad reaction from your plan or provider.
- Free to ask the Oregon Health Authority Ombudsperson for help with problems. They can be reached at 503-947-2346 or toll-free 877-642-0450 (TTY 711).
As an OHP member, you agree to:
- Find a doctor or other provider you can work with and tell them about your health.
- Treat providers and their staff with the same respect you want.
- Bring your Member ID card to appointments, tell the receptionist you have OHP and any other health insurance, and tell them if you were hurt in an accident.
- Be on time for appointments.
- Call your provider as soon as possible if you can’t make it to an appointment.
- Have yearly check-ups, wellness visits and other services to prevent illness and keep you healthy.
- Follow your providers’ and pharmacists’ directions or ask for another choice.
- Be honest with your providers to get the best service possible.
- Call OHP Customer Service when you move, are pregnant or no longer pregnant.
Columbia Pacific CCO takes fraud, waste and abuse seriously. We comply with all applicable laws, including the State and Federal False Claims Act. Examples of fraud, waste and abuse include:
Provider fraud:
- Billing for services not rendered
- Altering medical records
- Use of unlicensed staff
- Drug diversion (for example, dispensing substances with no medical purpose)
- Kickbacks and bribery
- Providing unnecessary services to members
Member fraud:
- Falsification of information
- Forging or selling prescription drugs
- Using transportation benefits for non-medical business
- Adding an ineligible dependent to the plan
- Lending or using another person’s insurance card
- Identity theft
The Oregon Health Authority (OHA) sends you a coverage letter that has your:
- Benefit package
- Coordinated care plan name
This letter shows information for everyone in your household who has an Oregon Health Plan (OHP) ID card. You do not need to take this letter to your health care appointments or to pharmacies. OHA will send you a new coverage letter if you ask for one or if your coverage changes.
OHA sends you one OHP ID card that has your name, Member ID number and the date the card was issued. All eligible members in your household receive their own OHP ID cards.
Keep your OHP ID card in a safe place. OHA only sends a new card if you change your name or ask for a new card. If your OHP ID card is not correct, or you get a new card with your name but a different Member ID, call OHP Customer Service right away at 800-699-9075 (TTY 711).
To keep your Oregon Health Plan coverage, you must re-apply every 12 months. OHP will send you a letter about how to keep your coverage.
There are three ways to contact OHP for questions or to make updates to your current information:
1. By telephone (toll-free): 800-699-9075
Members can call OHP to do any of the following:
- Change your address, phone number, family status, CCO or other information
- Replace a lost OHP Card
- Check the status of your application
- See if you or your children are still covered by OHP
- Change plans
- Solve a problem or make a complaint
- Get an OHP Handbook
2. By email: oregonhealthplan.changes@state.or.us When you write to this address, you must include your full name, date of birth, Member ID number and phone number.
Existing members can email OHP to change your address, phone number, family status, CCO or other information. PLEASE NOTE: the email address is for changes only.
3. Online: Most OHP members can report changes online at ONE.Oregon.gov. The online site supports the following browsers. (If you don't know your browser version, click your browser's Help menu, then click About.)
- Windows (PC): Internet Explorer 11, Internet Explorer 10, Internet Explorer 9, Internet Explorer 8, Firefox 39.0 and 43.0 and Chrome 43.0 and 44.0.
- Macintosh: Firefox 39.0 and 43.0 and Chrome 43.0 and 44.0. Safari is not supported.
- Smartphone browsers are not supported.
Need help?
- Learn how to set up your online account. English | Español
- Learn to use your online account dashboard. English | Español
- Watch a five-minute overview of the Applicant Portal.
OHP information for currently enrolled members:
If you are unhappy with Columbia Pacific CCO, your health care services or your provider, you can complain or file a grievance at any time, for anything other than a denial of service. Your provider or authorized representative may also file a grievance on your behalf with your written consent. We will try to make things better. Just call Customer Service at 855-722-8206, TTY 711, or send us a letter to the address on page 55 of your member handbook, available at the top of this page.
You can also fill out a complaint and feedback form here:
Columbia Pacific will work to resolve your complaint or grievance as quickly as your health condition requires. If we need more than five business days, we will send you a letter to let you know why. You will receive a final answer within 30 calendar days. We will not tell anyone about your complaint unless you ask us to.
You can also file a complaint with:
Oregon Health Authority (OHA)
Please call the OHP Client Services unit (CSU) toll free at 800-273-0557 or OHA's
Ombudsman at 503-947-2346 or toll free at 877-642-0450.
If we deny, stop or reduce a medical service your provider has ordered, we will mail you a Notice of Action letter explaining why we made that decision. You have a right to ask to change it through an appeal and a state fair hearing. You must ask for an appeal no more than 60 days from the date on the Notice of Action letter. You can ask for a denial notice that shows a service is not covered if:
- You did not receive a written notice of denial, or;
- Your provider tells you that you will need to pay for a service that is not covered.
For full instructions on the appeals process, please see page 54 of your member handbook, available at the top of this page.
Your provider has a right to appeal for you when their physician’s orders are denied by a plan. You must agree to this in writing. Instructions for this process can be found on page 55 of your member handbook.
