Columbia Pacific pays for many prescription drugs.
Columbia Pacific pays for many prescription drugs. The ones we cover are on a drug list called a “formulary.” When your provider prescribes a medicine, ask if it’s on the covered drug list. The list is a directory of medications approved for Columbia Pacific CCO members. It explains if there are special rules about the drug. The list is updated often, so if we remove or change a medication that you take, you’ll be notified in advance. To download and view the drug list, click the link below.
2025 Columbia Pacific CCO OHP Drug List (Formulary)
Download a machine-readable format (JSON) of the Formulary
OHP Prior Authorization Use criteria (updated 12/2025)
Member forms
Search for a drug in one of the following ways:
- Find the drug listed in the formulary/PDF index.
- In the PDF file, enter the drug name into the search box located in the menu.
- Call Customer Service for assistance in finding a drug.
If you want us to send you a printed copy of this formulary, please contact Customer Service. There is no charge, and you’ll receive it within five business days.
If you urgently need a drug that’s not on our formulary, call Customer Service. You, your provider or your pharmacist can ask for an emergency supply. The maximum emergency supply is 72 hours’ worth.
To fill a prescription, go to any pharmacy in our network. You’ll have lots of choices. Our network includes most large pharmacy chains and many smaller drug stores.
Mail-order pharmacies
You can have your drugs delivered directly to your door with one of our mail order pharmacies listed below. Click on the name of the pharmacy to open the form you'll need to fill out and send in.
New specialty pharmacy program
Columbia Pacific CCO is launching a new program to help Medicaid members who take certain specialty medications. Some specialty medications may now come from a different pharmacy that can better meet your needs. You can find a list of these medications here.
If your pharmacy changes, the new pharmacy will call you when you get a new prescription or need a refill. Your medication will stay the same. The name, brand, and amount will not change. If you already get your medication by mail, you can keep getting it that way. Your pharmacy benefits will not change.
For more information, see our FAQs below. For questions about the program, please call customer service at 855-722-8206 or TTY 711, Monday – Friday, 8 a.m. to 5 p.m.
MEDS Chart
It can be a real challenge keeping up with lots of prescriptions all at once. More and more people have ten, a dozen, 20 or more. It can be hard to keep them all straight, and even harder to tell your doctor when there’s something about your medications that you don’t like. CareOregon’s My Easy Drug System (MEDS) is a tested way to make sure your medications are working as a positive part of your health care plan.
The MEDS Chart helps you remember why you’re taking a medication, and let others know how you feel it’s working for you:
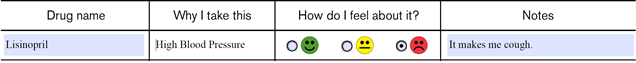
Download the MEDS Chart here
MEDS Chart Instructions - English
Alternate language options:
| Russian | Russian instructions |
| Spanish | Spanish instructions |
| Chinese | Chinese instructions |
| Vietnamese | Vietnamese instructions |
I have questions. How can I get help?
We’ll be happy to help you with your questions. Send us a secure message through the Member Portal. We will respond promptly.
